Oxford and Berlin join forces against dangerous germs
Two Cooperation Groups are dedicated to researching antibiotic resistance as part of the Grand Challenge Global Health
Feb 23, 2024
Global Health – the global fight against diseases and for better healthcare – is funded by the Berlin University Alliance as a “Grand Challenge” in numerous projects, including international ones. Part of this is also the the research on multi-resistant germs, to which millions of people fall victim year after year. Researchers from Berlin and Oxford are collaborating on two of these projects.
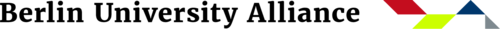
Many hospital infections are caused by methicillin-resistant Staphylococcus aureus strains - known as MRSA for short
Image Credit: National Institute of Allergy and Infectious Diseases/Unsplash
Globally, millions of people die every year from the consequences of an infection with multi-resistant germs. The risk of becoming infected either with bacteria that no longer respond to antibiotics or of contracting a fungal infection that can no longer be combated with antifungal drugs has been increasing for years. Researchers assume that by 2050, infections with antibiotic resistance will overtake cancer as a cause of human mortality.
Poor hygiene in hospitals or care facilities is the gateway for resistant bacteria, which result in the dreaded hospital-acquired infections. Nosocomial infections such as these include methicillin-resistant Staphylococcus aureus strains – abbreviated MRSA.
Grand Challenge Global Health: Oxford - Berlin
Two international research groups are searching for solutions to the decreasing effectiveness of antimicrobial drugs as part of the Oxford Berlin Research Partnership between the Berlin University Alliance (BUA) and the University of Oxford: they are investigating what role infection control and double infections through bacteria and fungi play in the development of antibiotic resistance. “Context-driven Infection Control Interventions” and “Bacterial-Fungal Co-Infections and their Role in the Evolution of Antimicrobial Resistance” are being funded for two years each by BUA as “Grand Challenge Global Health”. The funding is intended to make research results possible, on the basis of which the researchers will subsequently secure further, larger research grants.
What is special about the cooperation is that in each project, principal investigators (PIs) and postdocs in Oxford and Berlin work together on various aspects of the topic, thereby complementing each other with their expertise. Their aim is to contribute to containing multi-resistant germs.
Cooperation with Nigeria
Hygienic conditions are a key factor in the spread of multi-resistant germs in hospitals
Image Credit: Piron Guillaume/Unsplash
Cooperation with Nigeria
Countries in West Africa, south of the Sahara, are considered to be among the most affected by the consequences of multi-resistant germs. An international research group published a study on this in the medical journal “The Lancet” two years ago. According to this study, there were almost twice as many deaths per 100,000 people in the region as in rich industrialised countries.
The project “Context-Driven Infection Control Interventions” by the physicians PD Dr. med. Friederike Maechler (Charité) and Professor Christiane Dolecek as well as Professor Ben Cooper (Oxford) and Dr. Tochi Okwor (Nigeria) investigates the conditions under which multi-resistant germs spread in Nigerian hospitals in order to develop more effective monitoring strategies in the hospitals.
“Although there are already studies on hospital-acquired infections, they all refer to the occurrence of infection in so-called high-income countries in Europe or North America,” Friederike Maechler explains the initial position at the beginning of the project, which was launched in autumn 2021. By contrast, these study results have limited or no applicability to the situation in the low and middle-income countries of the so-called global South. The conditions in countries like Nigeria are completely different.
No access to water and electricity
“The mere fact that in many regions there is no electricity and insufficient access to water, creates different hygienic conditions,” Maechler emphasises. “And if even such basic things such as regular hand washing are not a matter of course, it becomes clear why many Nigerian hospitals are confronted with different challenges than, for instance, German ones, and why measures that are introduced in a German hospital make little sense in Nigeria.”
An additional problem is that hospital patients in Nigeria have to buy disinfectants or medicines themselves and bring them to the hospital. “Examinations like blood cultures, for example, must also be paid for by the patient. Blood cultures are very important for diagnostics, to determine the underlying bacterial pathogens and their resistance profile,” Christiane Dolecek adds. Moreover, there are too few microbiological laboratories in low and middle-income countries like Nigeria.
Expertise in surveillance research and infectiology
Friederike Maechler coordinates the surveillance surveys in the hospitals in Berlin at the Institute of Hygiene and Environmental Medicine. Dr. Tochi Okwor, public health expert from the Nigeria Centre for Disease Control (NCDC) and PI on the Nigerian side, also plays an important role in the project, as she has established an extensive surveillance network with her dedicated team, which is a cornerstone of the project’s success.
Dolecek and her colleague in Oxford, Ben Cooper, on the other hand, apply their profound expertise in infectiology with numerous survey studies on measures for handling multi-resistant germs to the project. Together, they manage the Global Research on Antimicrobial Resistance (GRAM) Project.
Hospitals in six different regions were selected, in the predominantly Muslim, poorer northern Nigeria, as well as in the predominantly Christian, economically better-off southern Nigeria. Medical staff were interviewed both on normal day wards and in intensive care units.
Several project workshops with the colleagues from Nigeria, as well as from six further African, Asian and European countries have already taken place in Berlin. They have strengthened existing contacts in all the participating countries and enlarged the network. Travel expenses and accommodation expenses for the team colleagues from Africa were able to be financed with BUA funds. “Our next step is to secure larger research grants on the basis of our results, in order to also continue the work beyond three years,” Christiane Dolecek says.
Interaction between bacteria and fungi
The declining effectiveness of antimicrobial and antifungal drugs is one of the biggest challenges in healthcare
Image Credit: Diana Polekhina/Unsplash
The second project “Bacterial-Fungal Co-Infections and their Role in the Evolution of Antimicrobial Resistance” takes account of the causes of the infections: the biology of the bacterium Pseudomonas aeruginosa, on the one hand, and the metabolism of fungi that cause infections in the human organism, on the other, and how they interact. Pseudomonas is among the most common causes of nosocomial infections worldwide. Patients are infected, for example, after surgery and contract wound or urinary tract infections or even pneumonia and sepsis.
The team on the BUA side is led by Professor Markus Ralser, Director of the Institute of Biochemistry at the Charité and previously research group leader at the Francis Crick Institute in London, and Dr. Lisa Kahl, postdoc and Marie Skłodowska-Curie Fellowship holder, at the same institute. The biochemists are experts in the field of cellular metabolism coordination and the development of analytical methods for working on complex biological questions.
In the project, the Charité side is focusing on fungal metabolism, while the partners in Oxford with Professor Craig McLean and postdoc Rachel Wheatley address the antibacterial drug resistance of Pseudomonas.
“We are investigating what role double infections through bacteria and fungi play in the development of antibiotic resistance, and are examining the genetics of the cells for this purpose,” Markus Ralser explains. “Generally, most fungal infections are namely not life-threatening for the human organism.”
If, however, an invasive infection is present – if, for example, the circulation or an organ is affected – the risk of a poor prognosis is very high. “The mechanisms of drug tolerance in fungi are also different from those in bacteria. While bacteria frequently develop genetic antibiotic resistance, this is rather rare in fungi. Fungi, however, develop non-genetic tolerances to antifungal drugs, and then no longer respond to these.”
Organism fights against two infections
The reality is, however, more complicated. The team established in laboratory experiments that Pseudomonas and fungi influence each other in resistance and tolerance. “Among fungi, in particular, it can be observed that their tolerance to antifungal drugs is increasing. And this is disastrous, considering that only three drug groups are currently available to treat fungal infections.”
If this happens, it is not only the antibiotic that encounters resistant bacteria, but also the fungi no longer respond to the antifungal agents, the human organism has to fight against two infections without effective antimicrobial “helpers”.
Ralser and his Oxford colleague also wish to secure subsequent grants after the BUA funding has ended, for the aim is clear: “We want to find out exactly how the exchange of information between the fungal and bacterial cells works – in order to contribute to the development of new drugs or to the further development of existing medicines with these findings.”
Further Information
The projects of the Oxford-Berlin cooperation described above are being funded by BUA with a total of 650,000 euros.
“Context-driven Infection Control Interventions”,
PI: PD Dr. med. Friederike Maechler (Charité – Universitätsmedizin Berlin), Prof. Christiane Dolecek (University of Oxford), Dr. Tochi Okwor (NCDC Nigeria), co-applicant: Prof. Joachim Trebbe (Freie Universität Berlin), Prof. Dr. Ben Cooper (University of Oxford), Dr. Tim Eckmanns (Robert Koch-Institut Berlin, RKI)
“Bacterial-Fungal Co-Infections and Their Role in the Evolution of Antimicrobial Resistance”, PI: Prof. Dr. Craig MacLean (University of Oxford), Prof. Dr. Markus Ralser (Charité – Universitätsmedizin Berlin), co-applicant: Dr. Rachel Wheatley (University of Oxford), Dr. Lisa Juliane Kahl (Charité – Universitätsmedizin Berlin), Dr. Federica Agostini (Charité – Universitätsmedizin Berlin)
Three further Cooperation Groups with the University of Oxford were supported with BUA funds. These are social science projects of “Grand Challenge Social Cohesion” that have already been completed:
“Fairwork”, BUA partners: Technische Universität Berlin and Humboldt-Universität; Transitions and Social Cohesion in the Context of Multiple Crises, BUA partner: Freie Universität Berlin; Oxford-Berlin Initiative on Museums as Spaces of Social Cohesion and Conflict, BUA partner: Technische Universität Berlin