The Simulated Human
On a new biotechnology and medical technology campus of Charité and Technische Universität Berlin, scientists from both institutions will be working on developing medical models based on the human body.
Jun 28, 2018
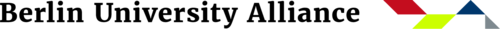
The “organ-on-a-chip” technology simulates the physiology and mechanics of organs, organ systems, or micro-scale tissues on chips the size of a playing card.
Image Credit: Anke Peters
The idea of using animals as models for the human body took hold about 100 years ago, when animal experiments prevailed for testing new drugs or therapies in medical research. This enabled important progress in research, in which Berlin scientists such as Robert Koch, Paul Ehrlich, Emil von Behring, and Otto Warburg played a major role. Scientists from Berlin have now set themselves the goal of developing new technologies that could make it possible to replace animal experiments in many areas with so-called human model systems.
To this end, Technische Universität Berlin and Charité – Universitätsmedizin Berlin – the medical school operated jointly by Freie Universität Berlin and Humboldt-Universität zu Berlin – are planning a joint research building, as recommended for funding by the German Council of Science and Humanities in April 2018 in the amount of 34 million euros. Within the framework of research buildings at universities and partly financed by the German Federal Government and the State of Berlin, the new building should be completed by 2023. The center will be jointly operated by Charité und Technische Universität Berlin in partnership.
“It’s exactly the right time to focus more on this experimental model.”
“Medicine is now being confronted with the great challenge of finding a solution for the time after antibiotics. As resistance to them is constantly rising, the end of this era is already in sight. In addition, cancer is still a major focus of medical research. The human immune system is the lynchpin of these diseases, which is why more and more researchers are focusing on immunotherapies,” says Prof. Dr. Andreas Thiel from the Berlin Brandenburg Center for Regenerative Therapies (BCRT) at Charité.
“The dilemma is that many of these new strategies can only be tested on humans, and of course that is not possible,” adds Prof. Dr. Roland Lauster, Head of Department for Medical Biotechnology at Technische Universität Berlin. The two scientists are the initiators of the planned “The Simulated Human” research project, abbreviated in German to “Si-M.”
Andreas Thiel is a professor of regenerative immunology and aging at the Berlin-Brandenburg Center for Regenerative Therapies (BCRT) of Charité - Universitätsmedizin Berlin.
Image Credit: Jacqueline Hirscher
“We now have methods at our disposal in medical biotechnology for cultivating and testing human cells and tissues which correspond to the conditions in the human body. According to Roland Lauster, “the time has come to focus on the simulated human as an experimental model.”
The scientists are currently concentrating on methods such as “organ-on-a-chip” technologies, 3D bioprinting, or even the most modern technologies of single cell analysis. The technology simulates the physiology and mechanics of organs, organ systems, or micro-scale tissues on chips the size of a playing card. These organ systems can be “placed” on the chip in different compartments. Integrated micropumps supply them with a nutrient solution or connect them together in such a way that cells can be exchanged.
In 3D bioprinting, on the other hand, printable biomaterials, so-called bioinks, and 3D printers are being developed with which functional 3D models of organs can be produced in mini-format.
Roland Lauster heads Medical Biotechnology at Technische Universität Berlin.
Image Credit: Ulrich Dahl - Stabsstelle Presse, Öffentlichkeitsarbeit und Alumni - Technische Universität Berlin
The third method, on which the scientists are currently working, is the latest method of single cell analysis. The technology uses the finding that both the genetic makeup and the presence of certain proteins in individual cells, for example from a blood sample, could provide early information about certain diseases; however, these findings are often lost when analyzing the entire sample. The trick in single cell analysis is, on the basis of various characteristics, to identify within a blood sample the few cells that are altered. In addition, by using multiple characteristics in different tissue samples, these methods make it possible to precisely identify individual cells. In this way, pathologically altered cells can be detected much earlier than previously possible.
“We now have methods at our disposal for cultivating and testing human cells and tissues which correspond to the conditions in the human body.”
The simple example of a sunburn shows what this can be good for: what happens in the body, which inflammatory processes take place, which cells, which reaction mechanisms are involved? As every sunburn causes irreversible damage, this can neither be tested on humans nor on animals. As the skin structure in humans and animals differs too much, there are also scientific reasons against doing this, in addition to ethical reasons. Modern-day procedures make it possible to cultivate, test, and analyze the skin organ, including its physiological environment.
The two professors, Roland Lauster and Andreas Thiel, developed the idea of joint research at the interface between engineering sciences at Technische Universität Berlin and medicine at Charité precisely with such visions in mind. Some of the new technologies, such as chip technology or 3D bioprinting, have been substantially developed or further developed at Technische Universität Berlin. These technologies are already being used to some extent in research projects, and the latest methods of single cell analysis are also being used for further investigations. In the Si-M joint science center, both institutions will not only collaborate but work side by side under one roof, thus opening up completely new possibilities in research on human models.
There is no shortage of potential joint projects between the two institutions. The application for the Si-M lists almost 50 planned cooperation projects. “Now it is important to start research as soon as possible so that the new research approaches can also lead to new diagnostic and therapeutic procedures. The results can be translated into real medical applications much faster than before,” says Andreas Thiel.
“The efficiency of new therapies can presumably be drastically increased, the side effects for patients minimized, and also the costs reduced.”
Any therapy which uses checkpoint blockade inhibitors is a good example of possible projects. These are used in immunotherapy for certain types of cancer. The patient is given a special antibody (a protein), the effect of which enables the body’s immune system to literally dissolve metastases and tumors. In some cancers, such therapies have achieved long-term cure rates of 30 to 40 percent. Problematic is that these antibodies interfere with the entire immune system, sometimes with considerable side effects, and they are extremely costly.
“Combining the technology of biotechnology at Technische Universität Berlin with the medical expertise at Charité, individual cancer cells could be taken from a biopsy to cultivate tumors on the chip under physiological conditions. Such tumors could be used to test which of the various new therapies works best to determine the most effective treatment for patients,” explains Andreas Thiel. “This could probably drastically increase the efficiency of the new therapies, minimize the side effects for patients, and also reduce the costs.”